High SGOT & SGPT: Causes, Diagnosis & Treatment
Understanding High SGOT and SGPT Levels: Causes, Diagnosis, and Next Steps
When your doctor orders a liver function test, you may see results for something called SGOT and SGPT. These two important markers can tell a lot about your liver health, but understanding what they mean isn't always straightforward.
SGOT (now commonly called AST) and SGPT (now commonly called ALT) are enzymes found primarily in your liver. When these enzymes show high levels in your bloodstream, it often signals that liver cells have been damaged and are leaking these enzymes into your blood. However, elevated levels don't always mean something serious - they could result from temporary issues, medication side effects, or even intense exercise.
Getting timely and accurate information about why your SGOT and SGPT levels are high is crucial for your health. Early diagnosis can mean the difference between a simple treatment plan and dealing with long-term liver complications. This comprehensive guide will walk you through everything you need to know about these important liver enzymes - what they are, what causes them to rise, how doctors diagnose the underlying issues, and what steps to take next.
What are SGOT (AST) and SGPT (ALT)?
Definitions and Basic Functions
SGOT (Serum Glutamic-Oxaloacetic Transaminase), now more commonly called AST (Aspartate Aminotransferase), is an enzyme found mostly in your liver, but also in your heart, muscles, kidneys, and brain. This enzyme helps in breaking down certain amino acids in your body.
SGPT (Serum Glutamic-Pyruvic Transaminase), now typically called ALT (Alanine Aminotransferase), is an enzyme primarily found in your liver cells. It's more specific to the liver than SGOT/AST, meaning high levels of SGPT/ALT are usually more indicative of liver problems.
Both these enzymes play important roles in metabolism, helping convert proteins into forms your body can use. They are normally contained within liver cells, but when liver cells are damaged, these enzymes leak into your bloodstream, causing elevated blood levels.
Normal Ranges for SGOT and SGPT
Normal ranges can vary slightly between different laboratories, but generally:
- SGOT/AST: 5 to 40 units per liter (U/L)
- SGPT/ALT: 7 to 56 units per liter (U/L)
Women and children may have slightly different normal ranges. It's always best to look at the specific reference ranges provided by the laboratory that performed your test.
Why These Enzymes Are Measured
Doctors measure SGOT and SGPT levels as part of routine liver function tests for several reasons:
- To screen for liver disease: Even before symptoms appear
- To monitor known liver conditions: Tracking how a liver disease is progressing or responding to treatment
- To assess liver damage: From medications, alcohol, or other substances
- To evaluate unexplained symptoms: Like jaundice, fatigue, or abdominal pain that might point to liver problems
- To monitor overall health: Sometimes as part of a comprehensive metabolic panel during regular check-ups
These tests are valuable because they're sensitive indicators of liver cell damage, often showing abnormalities before other signs of liver disease become apparent.
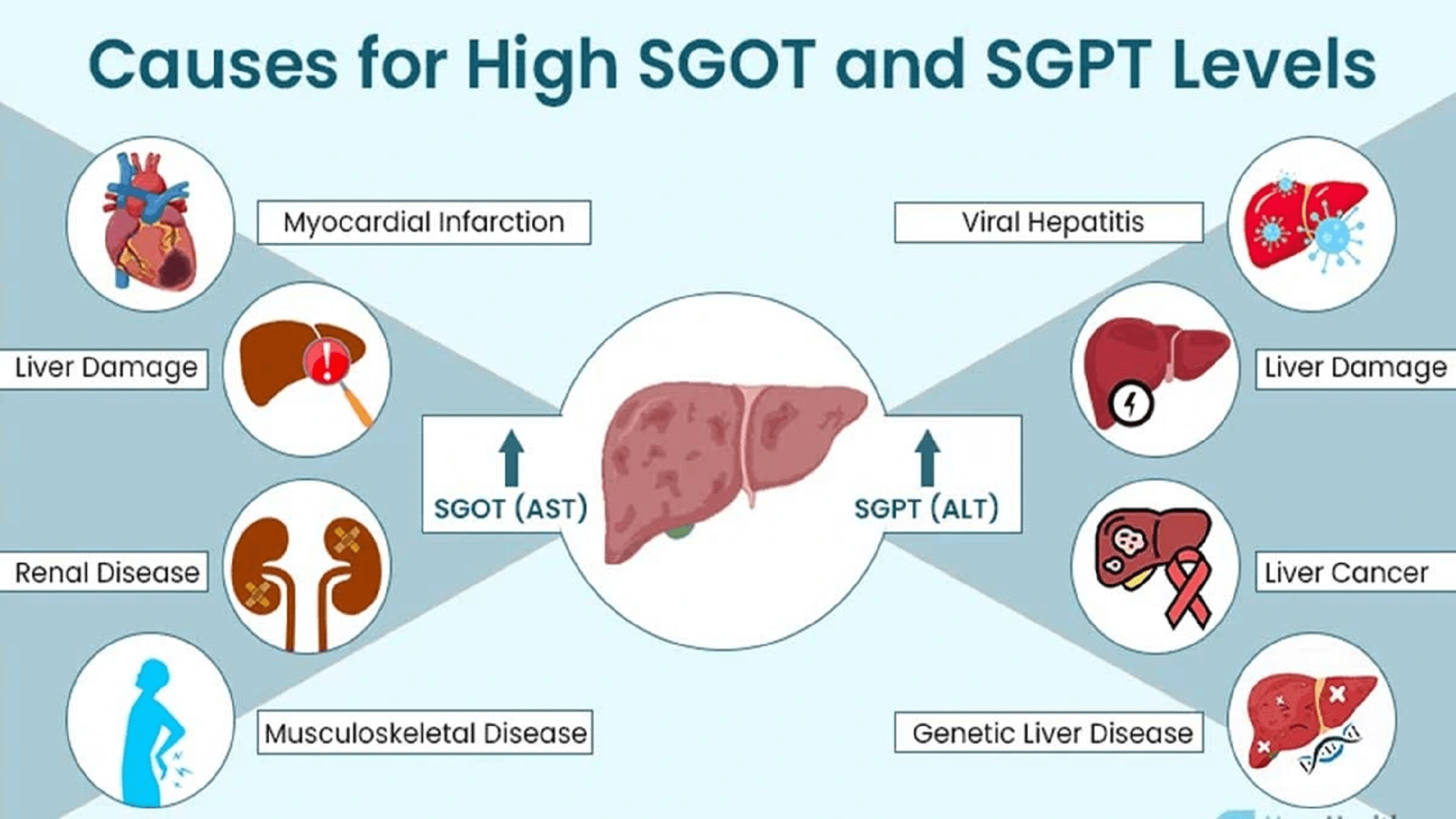
Causes of High SGOT and SGPT Levels
High levels of these liver enzymes can result from many different causes, both related to the liver and other parts of the body. Understanding what's behind elevated levels is key to proper treatment.
Liver-related Causes
Viral Hepatitis
Hepatitis viruses (A, B, C, D, and E) directly infect liver cells, causing inflammation and releasing SGOT and SGPT into the bloodstream. Hepatitis A and E are usually short-term infections, while B and C can become chronic and lead to long-term liver damage if not treated.
Alcoholic Liver Disease
Regular heavy drinking damages liver cells over time. This damage progresses from fatty liver to alcoholic hepatitis and eventually cirrhosis if drinking continues. SGOT levels are often higher than SGPT in alcoholic liver disease, usually with an AST/ALT ratio greater than 2:1.
Nonalcoholic Fatty Liver Disease (NAFLD)
This common condition affects people who drink little or no alcohol but develop fat deposits in their liver. It's closely linked to obesity, diabetes, and high cholesterol. In its more severe form, nonalcoholic steatohepatitis (NASH), inflammation and liver cell damage occur, raising enzyme levels.
Autoimmune Hepatitis
The body's immune system mistakenly attacks liver cells, causing ongoing inflammation and damage. This condition is more common in women and may be associated with other autoimmune disorders.
Liver Cirrhosis
Advanced scarring of the liver from various causes leads to cirrhosis. By this stage, SGOT and SGPT may actually be only mildly elevated or even normal because there are fewer healthy liver cells left to release these enzymes.
Liver Cancer (Hepatocellular Carcinoma)
Primary liver cancer can cause mild to moderate elevations in liver enzymes. Often, liver cancer develops in people who already have other liver conditions like cirrhosis or chronic hepatitis.
Drug-Induced Liver Injury (DILI)
Many medications can cause liver damage as a side effect. Common culprits include:
- Acetaminophen (especially in overdose)
- Certain antibiotics and antifungals
- Statins (cholesterol medications)
- Some anti-seizure medications
- Certain herbal supplements
Non-Liver Causes
Muscle Damage or Injury
Since SGOT/AST is also found in muscle tissue, any condition causing muscle damage can raise levels:
- Intense exercise or muscle strain
- Muscle trauma or crush injuries
- Muscular dystrophy
- Rhabdomyolysis (severe muscle breakdown)
Heart Conditions
During a heart attack (myocardial infarction), heart muscle cells die and release SGOT/AST into the bloodstream. Before specific heart tests were developed, doctors used SGOT levels to help diagnose heart attacks.
Pancreatitis
Inflammation of the pancreas can cause mild to moderate elevation of liver enzymes, especially when the inflamed pancreas is close to the liver.
Thyroid Disorders
Both hypothyroidism and hyperthyroidism can affect liver function and cause mild elevations in liver enzymes.
Hemolysis
When red blood cells break down in large numbers (hemolytic anemia), SGOT levels can rise.
Celiac Disease
This autoimmune reaction to gluten can sometimes cause elevated liver enzymes, which often return to normal on a gluten-free diet.
Certain Rare Genetic Disorders
Some inherited conditions can cause chronically elevated liver enzymes, such as Wilson's disease (copper accumulation) and hemochromatosis (iron overload).
SGOT and SGPT Elevated – What It Means Clinically
When your SGOT and SGPT levels come back high on a blood test, it's important to understand what these numbers actually mean for your health.
Interpreting Elevated Levels
The degree of elevation can provide clues about the underlying cause:
- Mild elevation (less than 5 times the upper limit of normal): Often seen in fatty liver disease, chronic hepatitis, or medication effects
- Moderate elevation (5-10 times normal): May indicate active hepatitis (viral or autoimmune), alcohol-related liver damage, or drug toxicity
- Severe elevation (more than 10 times normal): Typically points to acute injury such as viral hepatitis, drug-induced liver injury, or reduced blood flow to the liver
The AST/ALT Ratio (De Ritis Ratio)
The ratio between SGOT (AST) and SGPT (ALT) can help doctors determine the cause of liver damage:
- Ratio > 2:1 (AST much higher than ALT): Often seen in alcoholic liver disease, cirrhosis, or muscle damage
- Ratio < 1:1 (ALT higher than AST): Typical in viral hepatitis, nonalcoholic fatty liver disease, and many types of drug-induced liver injury
Acute vs. Chronic Liver Damage
Looking at enzyme patterns over time helps distinguish between:
- Acute liver damage: Sudden, sharp increases in enzymes, often reaching very high levels
- Chronic liver damage: Persistent mild to moderate elevations over months or years
In acute cases, levels typically rise quickly and then gradually return to normal as the liver heals. In chronic cases, levels may fluctuate but remain abnormal over long periods, indicating ongoing damage.
When to Be Concerned
Not all elevations require immediate concern. Factors that raise the level of concern include:
- Enzyme levels more than 3-5 times the upper limit of normal
- Elevations that persist over several tests
- Rising levels over time rather than stable or decreasing levels
- Accompanying symptoms like jaundice, abdominal pain, fatigue, or itching
- Other abnormal liver tests (bilirubin, albumin, prothrombin time)
- Risk factors for liver disease (heavy alcohol use, obesity, diabetes, hepatitis exposure)
Remember that context matters - a mild elevation in someone with multiple risk factors may be more concerning than a moderate elevation after intense exercise in an otherwise healthy person.
Diagnostic Approach for Elevated SGOT and SGPT Levels
When SGOT and SGPT levels are elevated, doctors follow a careful approach to find the underlying cause.
History and Physical Examination
Your doctor will start by asking detailed questions and examining you:
Medical History Questions
- Previous liver problems or hepatitis
- Alcohol consumption (amount, frequency, duration)
- Current medications including over-the-counter drugs and supplements
- Family history of liver disease
- Recent illnesses or infections
- Risk factors for viral hepatitis (travel history, needle exposure, etc.)
- Diet and weight changes
- Exercise habits, especially recent intense workouts
Physical Examination Focuses On
- Checking for jaundice (yellowing of skin or eyes)
- Feeling the liver to check for enlargement or tenderness
- Looking for signs of chronic liver disease like spider angiomas (small red spots on the skin) or palmer erythema (redness of the palms)
- Checking for fluid in the abdomen (ascites)
- Looking for swelling in the legs (edema)
Laboratory Tests
Based on initial findings, your doctor may order additional blood tests:
Comprehensive Liver Panel
- Bilirubin levels (direct and indirect): Elevated when the liver can't process bilirubin properly
- Alkaline phosphatase (ALP): Another liver enzyme that may indicate bile duct problems
- Gamma-glutamyl transferase (GGT): Helps distinguish liver disease from bone disease when ALP is elevated
- Albumin: Lower levels may indicate chronic liver damage affecting protein production
- Prothrombin time (PT) or INR: Measures blood clotting function, which can be impaired in liver disease
Viral Hepatitis Tests
- Hepatitis A antibodies (HAV IgM for recent infection)
- Hepatitis B surface antigen and antibodies
- Hepatitis C antibodies and RNA testing
- Less commonly, testing for hepatitis D or E
Autoimmune Markers
- Antinuclear antibodies (ANA)
- Smooth muscle antibodies (SMA)
- Liver-kidney microsomal type 1 (LKM-1) antibodies
- Immunoglobulin levels (IgG, IgM, IgA)
Other Specific Tests
- Iron studies (ferritin, transferrin saturation): For hemochromatosis
- Ceruloplasmin: For Wilson's disease
- Alpha-1 antitrypsin: For alpha-1 antitrypsin deficiency
- Creatine kinase (CK): To check for muscle damage as a cause of elevated SGOT/AST
- Lactate dehydrogenase (LDH): Another enzyme released during tissue damage
- Celiac disease antibodies: If celiac disease is suspected
- Thyroid function tests: To check for thyroid disorders
Imaging and Advanced Diagnostics
Liver Ultrasound
Usually the first imaging test, ultrasound can show fatty liver, liver size, gallstones, and some tumors. It's non-invasive and doesn't use radiation.
CT Scan
Provides more detailed images than ultrasound and can better detect liver tumors, abscesses, or vascular problems.
MRI and MRCP
Magnetic resonance imaging gives detailed pictures of the liver structure. MRCP (magnetic resonance cholangiopancreatography) specifically examines the bile ducts.
FibroScan (Transient Elastography)
A specialized ultrasound that measures liver stiffness to assess fibrosis (scarring) without an invasive biopsy.
Liver Biopsy
Though not always necessary, a liver biopsy provides the most definitive diagnosis. A small sample of liver tissue is removed with a needle and examined under a microscope. This is typically performed if:
- The diagnosis remains unclear after other tests
- The extent of damage needs to be precisely determined
- Treatment decisions depend on knowing the exact type and stage of liver disease
By following this systematic approach, doctors can usually identify the specific cause of elevated liver enzymes and develop an appropriate treatment plan.
Next Steps and Treatment Options
Once the cause of high SGOT and SGPT levels has been identified, treatment can begin. The approach varies widely depending on the underlying condition.
Addressing Specific Causes
Viral Hepatitis
- Hepatitis A and E: Usually resolve on their own with rest, adequate fluids, and proper nutrition
- Hepatitis B: May require antiviral medications like entecavir or tenofovir
- Hepatitis C: Highly effective direct-acting antiviral drugs can cure over 95% of infections
- Hepatitis D: More difficult to treat; may require pegylated interferon
Alcoholic Liver Disease
- Complete abstinence from alcohol is essential
- Nutritional support and vitamins, particularly B vitamins
- Medications to manage withdrawal symptoms if needed
- Support groups like Alcoholics Anonymous can help maintain sobriety
Nonalcoholic Fatty Liver Disease (NAFLD)
- Weight loss through diet and exercise (even 5-10% weight reduction helps)
- Control of diabetes and cholesterol
- Vitamin E may help in non-diabetic patients with proven NASH
- Medications like pioglitazone in certain cases
Autoimmune Hepatitis
- Corticosteroids like prednisone to reduce inflammation
- Immunosuppressants such as azathioprine for long-term management
- Regular monitoring of liver function and medication side effects
Drug-Induced Liver Injury
- Stopping the medication causing the problem
- Avoiding other potentially liver-toxic substances
- Supportive care while the liver heals
- In severe cases, N-acetylcysteine may be used
Other Specific Conditions
- Hemochromatosis: Phlebotomy (blood removal) to reduce iron levels
- Wilson's disease: Copper-binding medications like D-penicillamine
- Alpha-1 antitrypsin deficiency